| Drug Name | PTH-0366 |
| Description |
PTH-0366 is a recombinant form of human tissue kallikrein-1 (KLK1) that is being developed for the treatment of acute ischemic stroke. KLK1 enhances cerebral perfusion in ischemic areas by generating bradykinin, which is a peptide that induces vasodilation in the vascular system. Moreover, KLK1 can also promote angiogenesis. In the preclinical studies, PTH-0366 demonstrated good efficacy for improving brain tissue injury after cerebral infarction. |
| Target | Kallikrein 1 |
| Drug Modality | Recombinant protein |
| Indication | Acute ischemic stroke |
| Product Category | Signal transduction modulator |
| Mechanism of Action | Producing bradykinin for the potent local vasodilation |
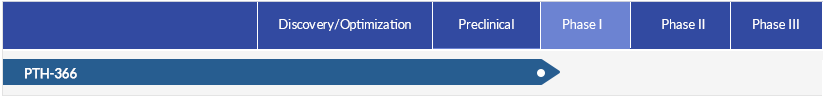
| Status | Phase I |
| Patent | Granted |
Protheragen Inc. is actively seeking partnership for PTH-0366. Potential collaboration can be strategic alliance, licensing, or marketing agreement.
We look forward to hearing from you.
| Introduction |
Kallikrein 1 (KLK1) is a single-chain acid glycoprotein consisting of 238 amino acids. The molecule is 25-45 kDa with isoleucine at amino terminal and serine at carboxyl terminal. KLK1 participates in protein hydrolysis that regulates various physiological processes. KLK1 mediates the formation of kinin from low molecular weight kallikreinogen (LMWK) through hydrolyzing one methionyl and one arginyl bond of domain 4 of LMWK. The kininase-kinin system is involved in various physiological and pathological functions, including inflammation, hypertension, kidney diseases, pancreatitis, and cancer. In addition, KLK1 can cleave insulinogen, low-density lipoprotein (LDL), the precursor of atrial natriuretic factor, prorenin, vasoactive intestinal peptide, procollagenase, and angiotensinogen. |
| Approved Name | Kallikrein 1 |
| Official Symbol | KLK1 |
| Gene Type | gene with protein product |
| Synonyms | Klk6 |
| Ensembl | ENSG00000167748 |
| Gene ID | 3816 |
| mRNA Refseq | NM_002257 |
| Protein Refseq | NP_002248 |
| OMIM | 147910 |
| UniProt ID | P06870 |
| Chromosome Location | 19q13.33 |
PTH-0366 is an active recombinant human KLK1 protein. The full-length preproprotein of human KLK1 is expressed in CHO cells, and then it is cleaved by recombinant trypsin to remove the pre-peptide sequence, resulting in the final target recombinant protein.
Stroke is an acute episode of focal dysfunction of the brain, spinal cord, or retinal cell death attributable to ischemia lasting long time. When a stroke occurs, those brain cells in the ischemic core undergo irreversible damage and are lost immediately. Other cells in the penumbra suffer acute damage and remain in a compromised state during a period of several hours. Cells in the penumbra are potentially salvageable but, in the absence of timely therapeutic intervention, are gradually recruited into the ischemic core.
Ischemic stroke is the main type of stroke caused by blockage, accounting for almost 80% of all cases. The other type is hemorrhagic stroke that caused by bleeding or hemorrhage such as an aneurysm in the brain or a head injury. According to the Global Burden of Disease (GBD) 2021 study, there were 93.8 million prevalent strokes and 11.9 million incident strokes worldwide in 2021. Overall, stroke was responsible for 15.2 million YLDs and 160.5 million DALYs globally that year. Also, according to GBD 2021, there were 69.9 million prevalent cases and 7.8 million incident cases of ischemic stroke worldwide that year. Due to the magnitude of aging populations and the increased prevalence of risk factors, increases are observed in the absolute number of incident and fatal strokes.
Kallikrein-1 (KLK1) is an enzyme that produces bradykinin, which offers a promising potential treatment for acute ischemic stroke. Studies have shown that the number of bombesin B2 receptors on the endothelial cells in the ischemic area of animals that suffered from acute stroke significantly increased. In this environment, the bradykinin produced by KLK1 would exert a potent local vasodilatory effect and increase cerebral perfusion through the downstream synergistic signaling pathways of the B2 receptors. Since KLK1 can preferentially act on the ischemic tissue, it can avoid systemic adverse reactions such as hypotension at an appropriate dose level. In addition, KLK1 can promote angiogenesis, forming new collateral vessels at the ischemic site for the improvement of regional blood flow to ischemic areas.
Therefore, PTH-366 may offer a new treatment option for acute ischemic stroke, with both rapid- and long-acting efficacy and improved prognosis.
In the preclinical studies, PTH-366 demonstrated excellent therapeutic effects in improving brain tissue injury after cerebral infarction, and showed favorable safety and PK profiles.