| Drug Name | RV-scFv-PDL1 |
| Description |
RV-scFv-PDL1 is the oncolytic rhabdovirus engineered with PD-L1 scFv. RV-scFv-PDL1 can be used to treat different types of cancer and can be easily modified or produced in large quantity. In mouse melanoma, lung cancer, colorectal cancer, and breast cancer models, RV-scFv-PDL1 showed inhibition in tumor growth. Mice survival rate has also increased greatly with treatment. No adverse effect was observed in rhesus monkeys after either intravenous or subcutaneous administration of RV-scFv-PDL1, ensuring its safety in primate. RV-scFv-PDL1 purification and production in small scale (for 50 patients) have been completed. |
| Indication | Melanoma, lung cancer, colorectal cancer, breast cancer, etc. |
| Target | PD-L1 |
| Oncolytic virus | Fusion protein |
| Mechanism of Action | In addition to directly lyse the tumor cells, RV-scFv-PDL1 also stimulates the immune system to kill tumor cells, as well as prevents the immune escape of tumor cells. |
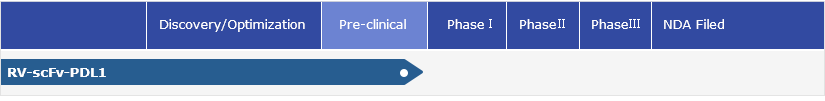
| Status | Preclinical |
| Patent | 1 international application submitted |
Protheragen Inc. is actively seeking partnership to further develop RV-scFv-PDL1. We look forward to collaborating with you soon.
| Introduction | TPD-L1 is a member of the B7 costimulatory family (immunoglobulin superfamily) that binds to PDCD1. It stimulates T-cell proliferation and induces the production of interleukin 10 and interferon gamma. Conversely, it inhibits T-cell responses in peripheral tissues by inducing apoptosis and arresting cell-cycle progression. |
| Approved Name | CD274 |
| Official Symbol | CD274 |
| Gene Type | Protein coding |
| Synonyms | B7-H; B7H1; PD-L1; PDL1; B7-H1 |
| Ensembl | ENSG00000120217 |
| Gene ID | 29126 |
| mRNA Refseq | NM_014143 |
| Protein Refseq | NP_054862.1 |
| OMIM | 605402 |
| UniProt ID | Q9NZQ7 |
| Chromosome Location | 9p24.1 |
| Gene Function |
Activation of human T cells and murine Pdcd1 +/+ T cells in the presence of PD-L1 led to a decrease in cell proliferation and cytokine secretion, possibly due to the presence of a cytoplasmic immunoreceptor tyrosine-based inhibitory motif (ITIM) on PDCD1. Using immunohistochemical analysis, B7H1 protein was found to be expressed in most human cancer cells but not in normal tissues. Cancer cell lines analyzed by flow cytometry showed upregulation of B7H1 expression in response to, but rarely in the absence of, IFNG. Expression of B7H1 from a melanoma cell line or a breast cancer-derived line, while in the absence of other apoptosis-inducing ligands, induced T-cell death through a receptor other than PD1. Apoptosis could be partially inhibited by neutralization of FASL (TNFSF6; 134638) and IL10. Cancer immunotherapy with preactivated T cells could be enhanced by blockade of B7H1. |
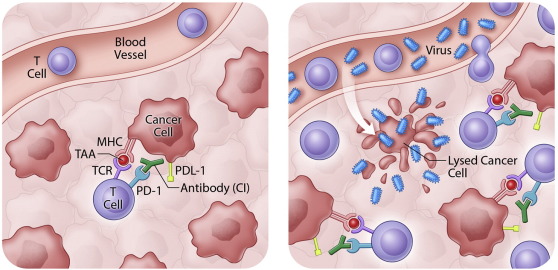
| Pathway | Engagement of PD-L1 with its receptor PD-1 on T cells delivers a signal that inhibits TCR-mediated activation of IL-2 production and T cell proliferation. |
| Major Conditions | Cancer; Gastrointestinal Disorders; Hematologic Diseases |
Oncolytic virotherapy is based on selective replication of viruses in cancer cells and their subsequent spread within a tumor microenvironment without causing damage to the surrounding normal tissue. Rv-scFv-PDL1 has been shown to inhibit tumor growth in several mouse tumor models, such as melanoma, lung and colorectal cancer.
| Melanoma |
Melanoma is a highly aggressive, therapy-resistant malignant tumor that originates in melanocytes, a specialized class of melanin-producing cells found primarily in the skin. The leading cause of death in melanoma patients is widespread metastases to the lymphatic system and other organs such as lung, liver, bone and brain. According to the International Agency for Research on Cancer (IARC)’s Globocan data for 2018, the global incidence of skin melanoma cases in 2018 was 287,723 and the five-year global prevalence was expected to be 965,623. The estimated global rate of mortality due to melanoma among males and females in 2018 was 34,831 and 25,881, respectively. |
| Lung cancer |
AThe two most common forms of lung cancer are non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC is further subdivided according to the type of cell in which the cancer develops into squamous cell carcinoma, adenocarcinoma, lung adenocarcinoma and large cell carcinoma, as well as more poorly differentiated variants. Unfortunately, many patients report a significant delay between emergence of symptoms and diagnosis of lung cancer. According to the IARC, lung cancer is the malignancy of highest impact in the world today, 2.1 million new cases (representing 11.6% of all new cancers) and 1.76 million in 2018 (equivalent to 18.4% of all cancer deaths). 1.185 million men and 576,000 women would die from lung cancer in 2018 worldwide, according to Globocan database. |
| Colorectal cancer |
Colorectal cancer is a heterogenous malignancy involving various molecular pathways and genetic/epigenetic alterations that trigger the sequential transformation of normal mucosa to adenoma and then to carcinoma. Colorectal cancer typically develops over a period of several years, progressing through various molecular and cytological stages before it becomes a carcinoma with the capacity for further invasion and metastasis. The global prevalence of colorectal cancer in 2018 was estimated at over 6.3 million, according to Globocan, with 1.8 million new cases predicted. Mortality rate caused by colorectal cancer has been estimated to be 880,792 worldwide in 2018. |
| Breast cancer |
Breast cancer is a type of cancer that specifically affects cells in the breast tissue. About 80% of breast cancers originate in the mammary ducts, while the remaining 20% originate in the lobules. According to the WHO, breast cancer is the most commonly diagnosed cancer in females worldwide, and the third most common cancer overall. In 2018, the IARC predicted that over two million would be diagnosed with breast cancer worldwide. In spite of a high treatment success rate, breast cancer remains the number one cause of cancer death for women, and the fifth most important cause of cancer death in both sexes combined. |
RV-scFv-PDL1 is the oncolytic rhabdovirus engineered with PD-L1 scFv. Oncolytic rhabdoviruses are natural pathogens but have been modified specifically to infect and destroy cancer cells. Infected cancer cells lead to an inflammatory response that produces cytokines. Some researchers also proposed that virus mediated tumor lysis leads to the release of tumor associated antigens and/or mutant proteins that stimulates therapeutically beneficial immune responses and results in T cell recruitment. However, these T cells then increase the expression of PD-L1 on cancer cells to induce immune inhibition. PD-L1 scFv can interrupt negative feedback systems within the tumor, effectively “taking the brakes off” pre-existing anti-tumor immune responses.
To summarize, infection of cancer cells by oncolytic rhabdovirus triggers induction of anti-tumor immunity and recruitment of T cells to tumors; addition of PD-L1 scFv ensures those T cells remain active. Therefore, RV-scFv-PDL1 can significantly improve the anti-tumor effect and reduce toxicity, compared to the combination of unmodified oncolytic virus and immune checkpoint inhibitors.
● Blocking amyloidogenesis by preventing β-amyloid precursor enzyme-1 (BACE1) expression and endocytosis;
● Blocking tau hyperphosphorylation induced by both Aβ and proneurotrophins.
 EBioMedicine 9 (2016) 31–36
EBioMedicine 9 (2016) 31–36
Currently, 1 international patent has been applied under PCT. In addition, purification and production of RV-scFv-PDL1 in small-scale (for 50 patients) have been completed. Preliminary safety assessments of RV-scFv-PDL1 in primates have been completed. No adverse reactions were observed.