| Drug Name | PTH-0300 |
| Description |
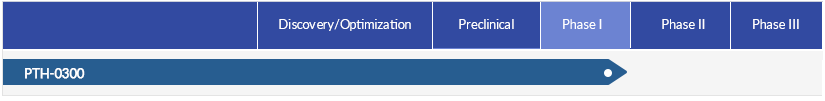
Epithelium-derived cytokine IL-25 is a central regulator for type 2 inflammation. PTH-0300 is a recombinant humanized IgG1 monoclonal antibody against IL-25, which is being developed for the treatment of type 2 inflammatory diseases. In healthy subjects, PTH-0300 showed favorable safety and pharmacokinetics profiles and a low immunogenicity. The clinical study report (CSR) of the Phase Ic clinical trial for asthma patients with PTH-0300 has been completed. In the United States and China, applications for Phase II clinical trials of PTH-0300 in patients with atopic dermatitis have been approved. Additionally, Phase II clinical trial applications for idiopathic pulmonary fibrosis (IPF) and chronic obstructive pulmonary disease (COPD) are currently underway. |
| Target | IL-25 |
| Drug Modality | Monoclonal antibody |
| Indication | Type 2 inflammatory diseases |
| Product Category | Immunotherapy |
| Mechanism of Action | Targeting IL-25 to reduce downstream mediators |
| Status | Phase II |
| Patent | Granted |
Protheragen Inc. is actively seeking partnership for PTH-0300. Potential collaboration can be strategic alliance, licensing, or marketing agreement.
We look forward to hearing from you.
| Introduction |
IL-25, also known as IL-17E, is one member of the IL-17 cytokine family that is associated with many immune regulatory effects and is associated with mediation of proinflammatory and allergic responses. IL-25 is an epithelial cell factor derived from epithelial tissues. Compared with other IL-17 cytokine family members, IL-25 shares relatively low sequence similarity with IL-17A and is functionally distinct from other IL-17 cytokines. The IL-25 receptor is a heterodimer composed of IL-17RB and IL-17RA. IL-25 mediates immune activity by binding to the IL-17RA/IL-17RB heteromeric receptor complex. As a proinflammatory cytokine, IL-25 aggravates allergic inflammation by promoting Th2 cells to produce IL-4, IL-5, IL-13 and other type 2 cytokines. |
| Approved Name | interleukin 25 |
| Official Symbol | IL25 |
| Gene Type | gene with protein product |
| Synonyms | IL-25; IL-17E |
| Ensembl | ENSG00000166090 |
| Gene ID | 64806 |
| mRNA Refseq | NM_022789 |
| Protein Refseq | NP_073626 |
| OMIM | 605658 |
| UniProt ID | Q9H293 |
| Chromosome Location | 14q11.2 |
| Pathway | T-helper 2 cell cytokine production; inflammatory response to antigenic stimulus |
| Major Conditions | Allergic asthma, psoriatic arthritis, melanoma, colorectal cancer, etc. |
PTH-0300 is a monoclonal antibody inhibitor specifically targeting IL-25. It inhibits the inflammatory response through blocking the binding of IL-25 to its receptor.
Type 2 inflammatory diseases are conditions characterized primarily by the secretion of type 2 cytokines and the infiltration of eosinophils. The pathophysiological mechanism of type 2 inflammation is driven by type 2 innate lymphoid (ILC2) cells and type 2 helper T (Th2) cells. Both ILC2 and Th2 cells produce type 2 cytokines, including interleukin (IL)-4, IL-5, and IL-13, which play multiple roles in the inflammatory cascade. Common type 2 inflammatory diseases include atopic dermatitis, asthma, allergic rhinitis, eosinophilic esophagitis, etc., involving multiple systems such as the skin, respiratory, and digestive systems, causing a heavy burden on patients.
| Atopic Dermatitis |
Atopic dermatitis (AD), also known as atopic eczema, is a chronic or chronically relapsing pruritic skin disease characterized by defects in the epidermal barrier. AD is considered an allergic disease resulting from genetic, environmental, immunologic and infectious factors as well as abnormal cutaneous barrier and decreased innate defenses. The condition affects approximately 129 million individuals worldwide, according to the Global Burden of Disease (GBD) study for 2021. The number of affected individuals is expected to reach 148 million in 2050, driven mostly by population growth. |
| Asthma |
Asthma is an immune-mediated inflammatory disease of the airway wall in which inflammation, goblet cell metaplasia, and physiological as well as pathological airway remodeling lead to bronchial smooth muscle hyperreactivity and airway obstruction. The disease is caused by interacting genetic and environmental factors, as well as abnormal immune maturation. Asthma is one of the leading causes worldwide of morbidity, health resource utilization and poor quality of life. According to the GBD study, there were about 260 million prevalent cases of asthma worldwide in 2021. This number is projected to reach 275 million in 2050. |
PTH-0300 is a monoclonal antibody specifically targeting IL-25, the key promoter of the type 2 immune response. The binding of IL-25 to its receptor IL-17RB/RA activates Th2 and ILC2 immune cells to initiate, amplify and maintain type 2 immune responses. Upregulation of IL-25 expression is often closely associated with type 2 immune responses in inflammatory diseases.
Inhibition of IL-25 may be a potential clinical treatment strategy for a variety of type 2 inflammatory diseases such as asthma, atopic dermatitis, and chronic sinusitis. In animal models of asthma, neutralizing antibodies to IL-25 significantly reduced bronchial hyperresponsiveness and inflammation, as well as improved histological features. The pharmacodynamic effects of IL-25 neutralizing antibodies also was showed in preclinical in vivo studies in atopic dermatitis.
The Phase Ic clinical trial in asthmatic patients demonstrated that the pharmacokinetic parameters and safety profile of PTH-0300 aligned closely with those observed in the Phase Ia/Ib studies conducted in healthy subjects. Furthermore, PTH-0300 exhibited a low immunogenicity risk profile across all study cohorts.
Applications for the Phase II clinical trials of PTH-0300 in patients with atopic dermatitis have been approved in the United States and China.
Safety: 40 healthy subjects were enrolled in Phase Ia SAD study (placebo, 0.5mg/kg, 1.67mg/kg, 3.34mg/kg, 5mg/kg, and 10 mg/kg), and 24 healthy subjects were enrolled in Phase lb MAD study (100mg/ 300mg/ 600mg/ placebo). There were no SAE or discontinuation due to an AE.
pharmacokinetics: In the Phase la study, the median Tmax was approximately 168 h (7 days) , the T1/2 ranged from 17.2 to 27.1 days, and the average MRT0-∞ was 29.2 to 35.4 days. The pharmacokinetic profile of PTH-0300 in the Phase lb study is similar to that in the Phase la study. The systemic exposure increased with the increase of dose, and the proportion of increase was slightly greater than the proportion to dose increase.